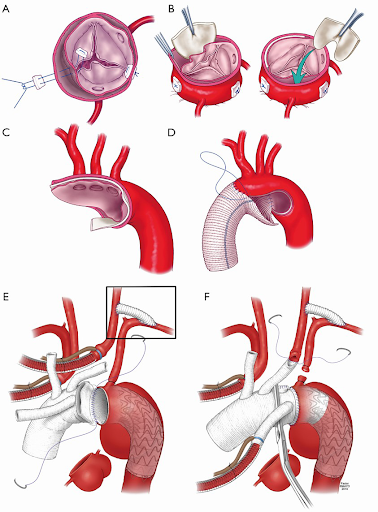
Patients who have an acute type A aortic dissection are a surgical emergency. Typically the ascending aorta is replaced with an open distal anastomosis such as a hemiarch with antegrade cerebral perfusion. The proximal anastomosis is then done at the sinotubular junction after removing all thrombus between the layers and gluing them together.
Approximately 31% of patients will require aortic root replacement as the dissection extends down into the sinuses and around the coronaries. As mentioned earlier, if the valve leaflets are normal then a valve-sparing root replacement is an option. The downside is an extended length of time during this critical operation, however with the proximal suture line below the annulus it may prevent bleeding. This is a major problem in patients with dissection. Because root replacement must be done in a significant proportion of Type A dissections there is incentive to understand outcomes in composite grafts versus stentless grafts. Lai et al examined their experience with Type A dissection patients who had AI and were stratified by root replacement with composite graft and separate valve graft. Composite grafts had slightly improved survival at long-term follow-up then did patients with a separate valve graft.
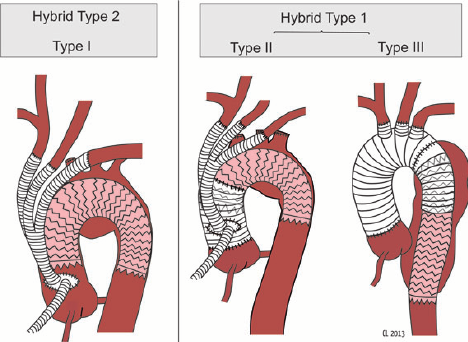
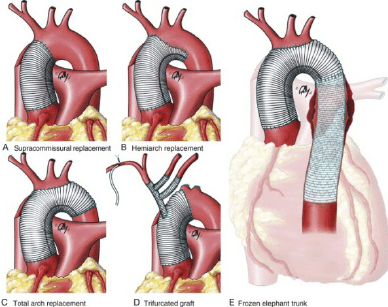
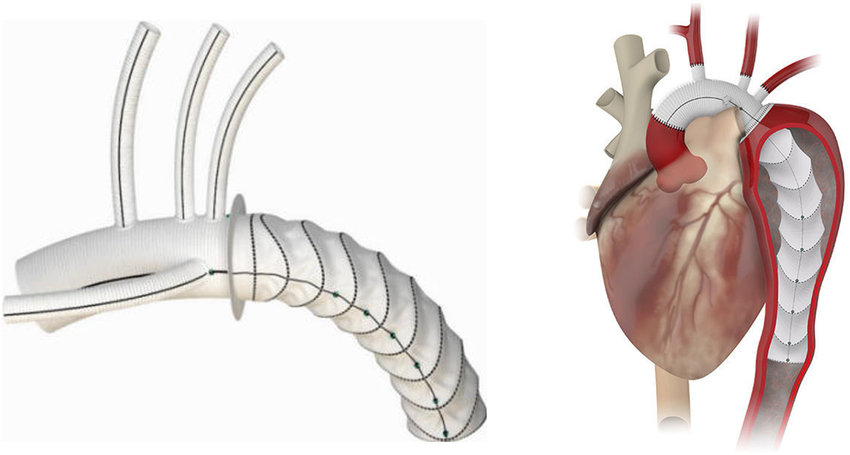
The arch of the aorta may also need to be repaired. This may also be done in conjunction with an elephant trunk procedure using hybrid techniques. Dr Babar Bashir CHAUDHRI is an expert in the repair of type A aortic dissections.