

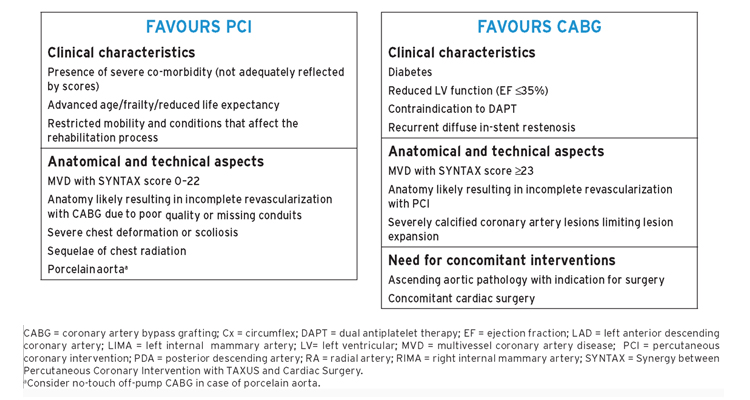
Aspects to be considered by the Heart Team for decision-making between percutaneous coronary intervention and coronary artery bypass grafting among patients with stable multivessel and/or left main coronary artery disease.
Revascularization with the use of coronary artery bypass grafting
The superiority of CABG over a strategy of initial medical therapy was established in a meta-analysis of seven RCTs68 more than two decades ago, demonstrating a survival benefit of CABG in patients with SCAD and left main (LM) or three-vessel disease, particularly when the proximal LAD coronary artery was involved, and has been corroborated in more recent studies.100,101 A network meta-analysis of 100 trials with 93 553 patients comparing a strategy of initial medical therapy with revascularization reported improved survival (RR 0.80, 95% CI 0.63–0.99) and a reduced risk of MI (RR 0.79, 95% CI 0.83–0.99) among patients undergoing CABG compared with initial medical treatment.100
In the STICH trial, 1212 patients with CAD and an LV ejection fraction (LVEF) ≤35% were randomized to initial medical therapy or CABG. The extended 10 year follow-up of the STICH trial reported a significant reduction in all-cause (59 vs. 66%; HR 0.84, 95% CI 0.73–0.97; P = 0.02) and cardiovascular mortality (41 vs. 49%; HR 0.79, 95% CI 0.66–0.93; P = 0.006).
Percutaneous coronary intervention vs. coronary artery bypass grafting
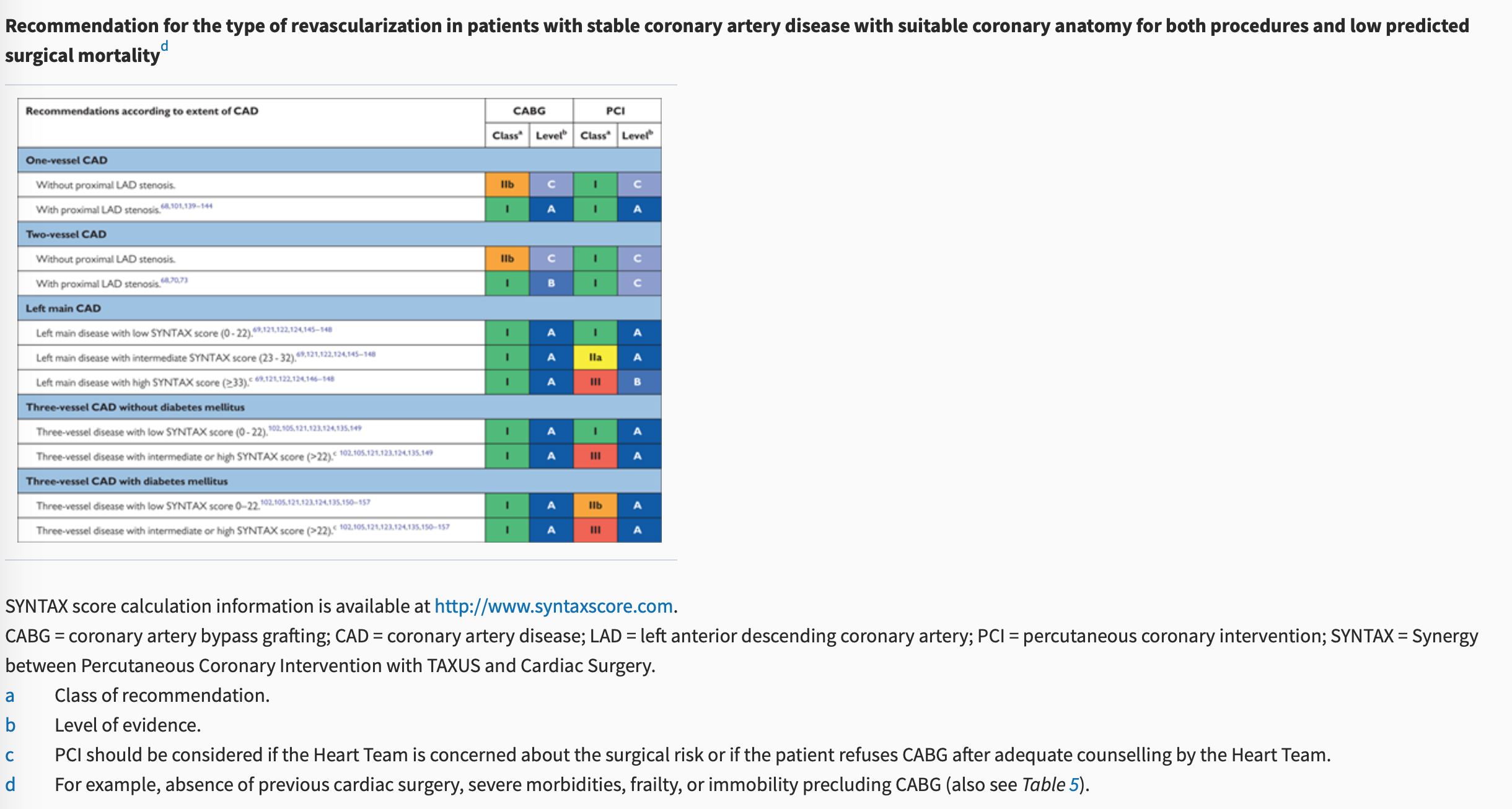
The recommendations for the type of revascularization (CABG or PCI) in patients with SCAD with suitable coronary anatomy for both procedures and low predicted surgical mortality are summarized below. The Heart Team should take into consideration the individual cardiac and extracardiac characteristics, in addition to patient preference, in the overall decision-making process.
Anatomical complexity of coronary artery disease
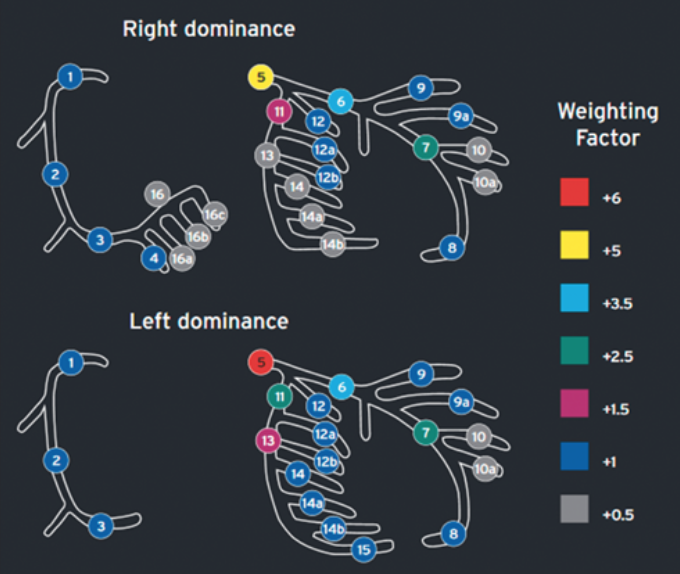
The SYNTAX score (http://www.syntaxscore.com) was prospectively developed for the SYNTAX trial to grade the anatomical complexity of coronary lesions in patients with LM or three-vessel disease. In the cohort of the SYNTAX trial, and subsequently in external validation cohorts, the SYNTAX score was found to be an independent predictor of long-term major adverse cardiac and cerebrovascular events (MACCE) and of death in patients treated with PCI but not CABG.
In the SYNTAX trial, tertiles of SYNTAX score with low, intermediate, and high anatomical complexity stratified patients into those who had similar outcomes with both PCI and CABG and those who derived significant benefit from CABG.121–123 In subsequent RCTs, the interaction of the strata of SYNTAX score with the effect of the randomized treatment was less pronounced and did not reach statistical significance.105–107 However, in a recent collaborative individual patient pooled analysis of randomized trials including 11 518 patients,124 the test for trend across the ordered tertiles of the SYNTAX score of the SYNTAX study was positive at P = 0.0011 (unpublished analysis), confirming the strata of the SYNTAX score as an effect modifier to be considered. There is concern about bias and inter-individual variability in calculating the SYNTAX score.125 This should be minimized by adequate training.
Completeness of revascularization
The aim of myocardial revascularization is to minimize residual ischaemia. In support of this concept, the nuclear substudy of the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) trial demonstrated an incremental benefit in reducing the risk of death and MI by reducing residual stress-induced ischaemia from >10% of the myocardium to ≤5%.86
In the SYNTAX trial, anatomical complete revascularization was defined as PCI or bypass of all epicardial vessels with a diameter exceeding ≥1.5 mm and a luminal reduction of ≥50% in at least one angiographic view.131 A meta-analysis of 89 883 patients enrolled in RCTs and observational studies revealed a lower long-term mortality (RR 0.71, 95% CI 0.65–0.77, P <0.001), MI (RR 0.78, 95% CI 0.68–0.90; P = 0.001), and repeat myocardial revascularization (RR 0.74, 95% CI 0.65–0.83; P<0.001) by complete revascularization (based on anatomical definition in 87% of the patients) as compared with incomplete revascularization.132 The benefit of complete revascularization was independent of the treatment modality. A more recent meta-analysis suggested enhanced benefit when complete revascularization is performed with state-of-the-art techniques in high-risk patients.133Likewise, in a post hoc analysis of the SYNTAX trial, anatomical incomplete revascularization was associated with inferior long-term outcomes after both CABG and PCI.131 A residual SYNTAX score >8 after PCI was associated with significant increases in the 5-year risk of death and of the composite of death, MI, and stroke, and any residual SYNTAX score >0 was associated with the risk of repeat intervention.134 In an observational study from the New York State registry that compared CABG with PCI using new-generation Stent in 9223 pairs of propensity-matched patients with multivessel CAD, the significantly higher risk of MI associated with PCI as compared with CABG was not seen among matched pairs of patients in which the PCI group had complete revascularization (Pinteraction = 0.02).135Consistent findings were obtained in a pooled analysis of 3212 patients of the SYNTAX, BEST (Randomised Comparison of Coronary Artery Bypass Surgery and Stent Implantation in the Treatment of Patients with Multivessel Coronary Artery Disease), and PRECOMBAT (Premier of Randomised Comparison of Bypass Surgery versus Angioplasty Using Stents in Patients with Left Main Coronary Artery Disease) trials.136 A mean SYNTAX score of 27 and an LVEF of 59% were obtained. In a propensity-matched analysis, mortality and the composite risk of death, MI, and stroke were significantly lower after PCI with complete vs. incomplete revascularization. After PCI with complete revascularization, the risk of death or of the composite of death, MI, or stroke was not significantly different from that after CABG with complete revascularization (adjusted HR 1.16, 95% CI 0.83–1.63, P = 0.39, and 1.14, 95% CI 0.87–1.48, P = 0.35, respectively), whereas these risks were significantly elevated after PCI with incomplete revascularization.
Functional complete revascularization is achieved when all lesions causing resting or stress-induced ischaemia are bypassed or treated by PCI. Given the limitations of non-invasive imaging techniques (see section 3), these lesions are identified by FFR or iwFR during diagnostic angiography. For PCI, the FAME study demonstrated that the more restrictive selection of target lesions by functional guidance conferred superior long-term outcomes compared with anatomically guided lesion selection (see section 3).31 In contrast, leaving functionally relevant lesions untreated resulted in a high rate of reinterventions in the FAME 2 study.33 Based on the data of the FAME and FAME 2 studies, complete revascularization based on the functional definition is the preferred strategy for PCI.
The role of functional guidance for CABG is less clear.28,137 One of the potential benefits of CABG is protection against disease progression in proximal segments, which may be diminished by restricting the bypass targets to functionally relevant lesions. This has to be weighed against the risk of bypass closure when native vessel flow is high. Thus, for ambiguous lesions, functional testing may also help guide the surgical revascularization strategy.
Isolated proximal left anterior descending coronary artery disease
Comparing CABG and PCI among patients with isolated proximal LAD disease, the available evidence suggests similar outcomes in terms of death, MI, and stroke, but a higher risk of repeat revascularization with PCI.
Left main coronary artery disease
The available evidence from RCTs and meta-analyses comparing CABG with PCI using DES among patients with LM disease suggests equivalent results for the safety composite of death, MI, and stroke up to 5 years of follow-up.148 A significant interaction with time is notable, providing early benefit for PCI in terms of MI and peri-interventional stroke, which is subsequently offset by a higher risk of spontaneous MI during long-term follow-up. The need for repeat revascularization is higher with PCI than with CABG.
The EXCEL trial compared CABG with PCI using new-generation DES (EES) among 1905 patients with significant LM disease.107 At 3 years of follow-up, the primary endpoint of death, stroke, or MI occurred with similar frequency in the CABG and PCI group (14.7 vs. 15.4%; HR 1.00, 95% CI 0.79–1.26, P = 0.98). The pre-planned landmark analysis from 30 days to 3 years showed a significant difference for the primary endpoint in favour of CABG (7.9 vs. 11.5%, P = 0.02).
The NOBLE (Nordic-Baltic-British Left Main Revascularization Study) trial compared CABG with PCI using new-generation DES [biolimus-eluting stents (BES)] among 1201 patients with significant LM disease (mean SYNTAX score of 23).106 At a median follow-up of 3.1 years, the primary endpoint of death, non-procedural MI, stroke, and repeat revascularization occurred more frequently in the PCI than the CABG group (29 vs. 19%; HR 1.48, 95% CI 1.11–1.96, P = 0.007).
A recent collaborative individual patient pooled analysis of randomized trials including 11 518 patients reviewed the currently available evidence from randomized trials comparing CABG with PCI for LM or multivessel disease.124 The primary outcome was all-cause mortality. In the overall cohort, CABG was associated with a significant survival benefit during a mean follow-up of 3.8 ± 1.4 years (5 year all-cause mortality 11.2% after PCI vs. 9.2% after CABG; HR 1.20, 95% CI 1.06–1.37, P = 0.0038). There was a linear trend for HRs of death increasing with increasing SYNTAX tertiles [P = 0.0011 for trend (unpublished analysis)]. However, among 4478 patients with LM disease, those randomly assigned to CABG or PCI with a mean follow-up of 3.4 ± 1.4 years reported similar risks for the primary outcome all-cause mortality (PCI 10.7 vs. CABG 10.5%; HR 1.07, 95% CI 0.87–1.33, P = 0.52) at 5 years. There were no significant differences in mortality between PCI and CABG in subgroup analyses according to SYNTAX scores. Nevertheless, in patients with a high SYNTAX score, a trend towards better survival was noted with CABG. The proportion of patients with a high SYNTAX score was limited in view of the inclusion criteria of the respective studies.
Current evidence indicates that PCI is an appropriate alternative to CABG in LM disease and low-to-intermediate anatomical complexity. Among patients with LM disease and low anatomical complexity, there is evidence that the outcomes with respect to major clinical endpoints are similar for PCI and CABG, resulting in a class I recommendation. Among patients with LM disease and high anatomical complexity, the number of patients studied in RCTs is low due to exclusion criteria; the risk estimates and CIs are imprecise, but suggest a trend towards better survival with CABG. Therefore, PCI in this setting cannot be endorsed as reflected by a class III recommendation. For PCI in LM with intermediate anatomical complexity, the previous class IIa recommendation was maintained in view of the incomplete 5 year follow-up of the two largest RCTs in this setting.
Multivessel coronary artery disease
The observation of a survival advantage of CABG over PCI has been consistent among patients with severe three-vessel CAD (intermediate to high SYNTAX score), and has been attributed at least in part to the placement of bypass grafts to the mid coronary vessels providing prophylaxis against the development of new proximal disease.
The BEST trial, comparing CABG with PCI using new-generation DES (EES) among patients with multivessel CAD (77% three-vessel CAD and 23% two-vessel disease, mean SYNTAX score 24), prematurely stopped enrolment after the inclusion of 880 patients due to slow recruitment.105 At a median follow-up of 4.6 years, PCI was associated with a higher incidence of the primary endpoint (death, MI, and TVR) (15.3 vs. 10.6%; HR 1.47, 95% CI 1.01–2.13, P = 0.04) than CABG. The risk of death, MI, and stroke was not statistically different between the two treatment groups (11.9 vs. 9.5%; HR 1.26, 95% CI 0.84–1.89, P = 0.26), whereas repeat revascularization of any vessel (11.0 vs. 5.4%; HR 2.1, 95% CI 1.28–3.41, P = 0.003) but not target lesion revascularization (5.7 vs. 3.8%; HR 1.51, 95% CI 0.82–2.80, P = 0.19) was more frequent in the PCI group. CABG resulted in more complete revascularization (71.5 vs. 50.9%; P <0.001) and a lower incidence of revascularization for new lesions (5.5 vs. 2.3%; HR 2.47, 95% CI 1.18–5.17, P = 0.01).
Consistent with findings in the overall cohort (see section 5.3.3), the collaborative individual patient pooled analysis found that in 7040 patients with multivessel disease, those assigned to CABG had significantly lower 5 year all-cause mortality than those assigned to PCI (PCI 11.5 vs. CABG 8.9%; HR 1.28, 95% CI 1.09–1.49, P = 0.0019).124 Outcomes for the endpoint all-cause mortality were modified by two variables, diabetes and disease complexity, as assessed by the SYNTAX score. Compared with patients without diabetes (8.7 vs. 8.0%; HR 1.08, 95% CI 0.86–1.36, P = 0.49), mortality was higher after PCI than CABG in patients with diabetes (15.5 vs. 10.0%; HR 1.48, 95% CI 1.19–1.84, P = 0.0004, Pinteraction = 0.045). There was a gradient of risk with a stepwise increase in mortality for PCI according to SYNTAX score tertile (SYNTAX score 0 − 22: 10.5 vs. 8.4%; HR 1.11, 95% CI 0.77–1.62, P = 0.57; SYNTAX score 23 − 32: 14.0 vs. 9.5%; HR 1.50, 95% CI 1.09–2.08, P =0.0129; SYNTAX score >32: 19.2 vs. 11.2%; HR 1.70, 95% CI 1.13–2.55, P = 0.0094).
An individual patient data pooled analysis of SYNTAX and BEST, comparing CABG with PCI using DES among 1275 patients with multivessel disease in the absence of diabetes (89% three-vessel CAD, mean SYNTAX score 26), reported a lower risk of death (6.0 vs. 9.3%; HR 0.65, 95% CI 0.43–0.98, P = 0.04) and MI (3.3 vs. 8.3%; HR 0.40, 95% CI 0.24–0.65, P <0.001) in the CABG group at a median follow-up of 61 months.149 The risk of death was not significantly different among patients with a low (0 − 22) SYNTAX score (6.0 vs. 7.5%, P = 0.66), whereas the benefit of CABG over PCI was greater in patients with an intermediate-to-high (>22) SYNTAX score (7.1 vs. 11.6%, P = 0.02). Another individual patient data pooled analysis of SYNTAX and BEST, comparing CABG with PCI using DES among 1166 patients with multivessel disease involving the proximal LAD (88% three-vessel CAD, mean SYNTAX score 28), reported a higher risk of the composite of death, MI, and stroke (16.3 vs. 11.5%; HR 1.43, 95% CI 1.05–1.96, P = 0.02), cardiac death, MI, and repeat revascularization in the PCI group at 5 years of follow-up.147 Of note, outcomes were not significantly different for CABG and PCI for any endpoint except for MI among the subgroup of patients with low SYNTAX score (0 − 22).
The available evidence suggests that in multivessel CAD without diabetes and low anatomical complexity, PCI and CABG achieve similar long-term outcomes with respect to survival and the composite of death, MI, and stroke, justifying a class I recommendation for PCI. In patients with multivessel CAD and intermediate-to-high anatomical complexity, the two large trials using DES, SYNTAX and BEST, found a significantly higher mortality and a higher incidence of death, MI, and stroke with PCI in the absence of diabetes. Consistent results were also obtained for patients with multivessel CAD in the recent individual patient-level meta-analysis.124 Thus, the previous class III recommendation for PCI in multivessel CAD and intermediate-to-high complexity was maintained.